Achieving Excellence: The Power of Patient Care Coordination in Healthcare
Patient Care Coordination: Enhancing Healthcare Delivery
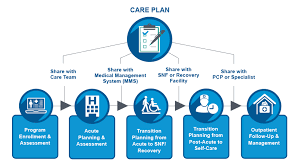
In today’s complex healthcare landscape, patient care coordination plays a vital role in ensuring seamless and efficient delivery of healthcare services. It involves the systematic organization, communication, and collaboration among healthcare providers to meet the diverse needs of patients.
Effective patient care coordination is essential for several reasons. Firstly, it improves patient outcomes by ensuring that all healthcare professionals involved in a patient’s care are well-informed and working together towards a common goal. This reduces the likelihood of medical errors, duplicate tests, and conflicting treatment plans.
Furthermore, care coordination enhances patient satisfaction. By streamlining the healthcare process and minimizing delays or unnecessary steps, patients experience smoother transitions between different providers and settings. This results in improved continuity of care, reduced stress levels, and increased trust in the healthcare system.
One crucial aspect of care coordination is effective communication. Health information exchange between different providers allows for a comprehensive understanding of a patient’s medical history, current conditions, medications, and treatment plans. This facilitates better decision-making and enables healthcare professionals to provide personalized care that aligns with the individual needs of each patient.
Technology plays a significant role in supporting patient care coordination efforts. Electronic health records (EHRs), for instance, provide a centralized platform where medical information can be securely stored and accessed by authorized providers. EHR systems allow for real-time updates on patients’ health status, ensuring that all relevant parties have access to the most up-to-date information.
Additionally, telemedicine has emerged as an invaluable tool for care coordination, particularly in remote or underserved areas. Through virtual consultations and remote monitoring devices, healthcare professionals can collaborate with specialists or provide ongoing support to patients without requiring them to travel long distances.
A successful patient care coordination model also involves engaging patients as active participants in their own care. By providing education, clear instructions, and involving them in shared decision-making, patients become empowered to manage their health effectively. This collaborative approach fosters a sense of ownership and accountability, leading to improved treatment adherence and better health outcomes.
Ultimately, patient care coordination is an ongoing process that requires commitment and collaboration from all stakeholders involved in healthcare delivery. Healthcare providers, administrators, policymakers, and patients must work together to implement strategies that prioritize effective communication, streamlined workflows, and patient-centered care.
By embracing patient care coordination as a fundamental aspect of healthcare delivery, we can enhance the overall quality of care while reducing costs and improving patient satisfaction. Together, let us strive for a healthcare system that seamlessly coordinates services with the ultimate goal of improving the health and well-being of every individual.
8 Essential Strategies for Effective Patient Care Coordination
- Maintain open and clear communication with patients and their caregivers.
- Ensure that all relevant medical information is accurately documented and shared among healthcare providers.
- Coordinate appointments, tests, and treatments to minimize delays or conflicts.
- Facilitate collaboration between different healthcare professionals involved in a patient’s care.
- Educate patients about their conditions, treatment plans, and self-care strategies.
- Advocate for patients’ needs and preferences within the healthcare system.
- Promote continuity of care by following up on treatment progress and addressing any concerns or changes in condition.
- Engage patients in shared decision-making processes to empower them to actively participate in their own care.
Maintain open and clear communication with patients and their caregivers.
Maintaining open and clear communication with patients and their caregivers is a vital aspect of patient care coordination. Effective communication ensures that everyone involved in a patient’s care is well-informed, understands the treatment plan, and can actively participate in decision-making. By actively listening to patients and their caregivers, healthcare providers can address concerns, provide necessary information, and establish trust. Clear communication also helps prevent misunderstandings, reduces anxiety, and fosters a collaborative environment where patients feel empowered to actively engage in their own care. Ultimately, open and transparent communication strengthens the patient-provider relationship and enhances the overall coordination of care for better health outcomes.
Ensure that all relevant medical information is accurately documented and shared among healthcare providers.
Accurate documentation and sharing of relevant medical information among healthcare providers is a crucial aspect of patient care coordination. By ensuring that all pertinent details, such as medical history, test results, diagnoses, and treatment plans, are accurately recorded and readily accessible to authorized professionals, we can facilitate effective collaboration and decision-making. This practice minimizes the risk of errors, improves continuity of care, and ensures that each healthcare provider has a comprehensive understanding of the patient’s condition. Through meticulous documentation and seamless information exchange, we can enhance the quality of care provided and ultimately contribute to better patient outcomes.
Coordinate appointments, tests, and treatments to minimize delays or conflicts.
In the realm of patient care coordination, one crucial tip is to coordinate appointments, tests, and treatments effectively to minimize delays or conflicts. By carefully scheduling and synchronizing these various aspects of healthcare, we can ensure that patients receive timely and efficient care without unnecessary waiting periods or overlapping procedures. This approach not only optimizes the use of healthcare resources but also enhances patient satisfaction by reducing frustration and streamlining their overall healthcare experience. By prioritizing coordination in scheduling, we can provide patients with a seamless journey through their healthcare journey while maximizing the effectiveness of their treatments and interventions.
Facilitate collaboration between different healthcare professionals involved in a patient’s care.
Facilitating collaboration between different healthcare professionals involved in a patient’s care is a crucial aspect of effective patient care coordination. By promoting open communication and information sharing, healthcare providers can work together as a cohesive team to ensure that the patient receives comprehensive and coordinated care. This collaboration allows for the exchange of valuable insights, expertise, and perspectives, leading to better decision-making and improved patient outcomes. By fostering a culture of collaboration, healthcare professionals can collectively address complex medical issues, avoid duplication of efforts, and provide seamless care transitions for the benefit of the patient.
Educate patients about their conditions, treatment plans, and self-care strategies.
Educating patients about their conditions, treatment plans, and self-care strategies is a crucial aspect of patient care coordination. By providing comprehensive information and clear explanations, healthcare providers empower patients to actively participate in their own care. When patients are well-informed about their conditions and treatment options, they can make informed decisions and take necessary steps to manage their health effectively. Moreover, educating patients about self-care strategies equips them with the knowledge and skills to prevent complications, adhere to treatment regimens, and promote overall well-being. This collaborative approach fosters a sense of partnership between healthcare providers and patients, leading to improved outcomes and patient satisfaction.
Advocate for patients’ needs and preferences within the healthcare system.
Advocating for patients’ needs and preferences within the healthcare system is a crucial aspect of effective patient care coordination. As healthcare professionals, it is essential to actively listen to patients, understand their unique circumstances, and ensure that their voices are heard. By advocating for patients, we can help bridge the gap between their needs and the healthcare system, ensuring that they receive personalized care that aligns with their preferences. This involves communicating with other providers, coordinating services, and addressing any barriers or challenges that may arise. Ultimately, patient advocacy empowers individuals to actively participate in their own care and promotes a patient-centered approach to healthcare delivery.
Promote continuity of care by following up on treatment progress and addressing any concerns or changes in condition.
Promoting continuity of care is a crucial aspect of patient care coordination. By actively following up on treatment progress and addressing any concerns or changes in a patient’s condition, healthcare providers can ensure that the care provided remains effective and tailored to the individual’s needs. Regular check-ins, monitoring of symptoms, and open communication channels allow for timely interventions and adjustments to treatment plans. This proactive approach not only enhances patient outcomes but also fosters trust and confidence in the healthcare team, empowering patients to actively participate in their own care journey.
Engage patients in shared decision-making processes to empower them to actively participate in their own care.
Engaging patients in shared decision-making processes is a crucial tip for effective patient care coordination. By involving patients in the decision-making process, healthcare providers empower them to actively participate in their own care. This approach recognizes that patients have unique insights into their health, preferences, and values. When patients are informed about their treatment options and actively involved in making decisions, they become more engaged and motivated to follow through with their treatment plans. This collaborative approach not only improves patient satisfaction but also leads to better treatment adherence and ultimately, improved health outcomes.
