Understanding the Importance of Advance Medical Directives in Healthcare Decision-Making
The Importance of Advance Medical Directives
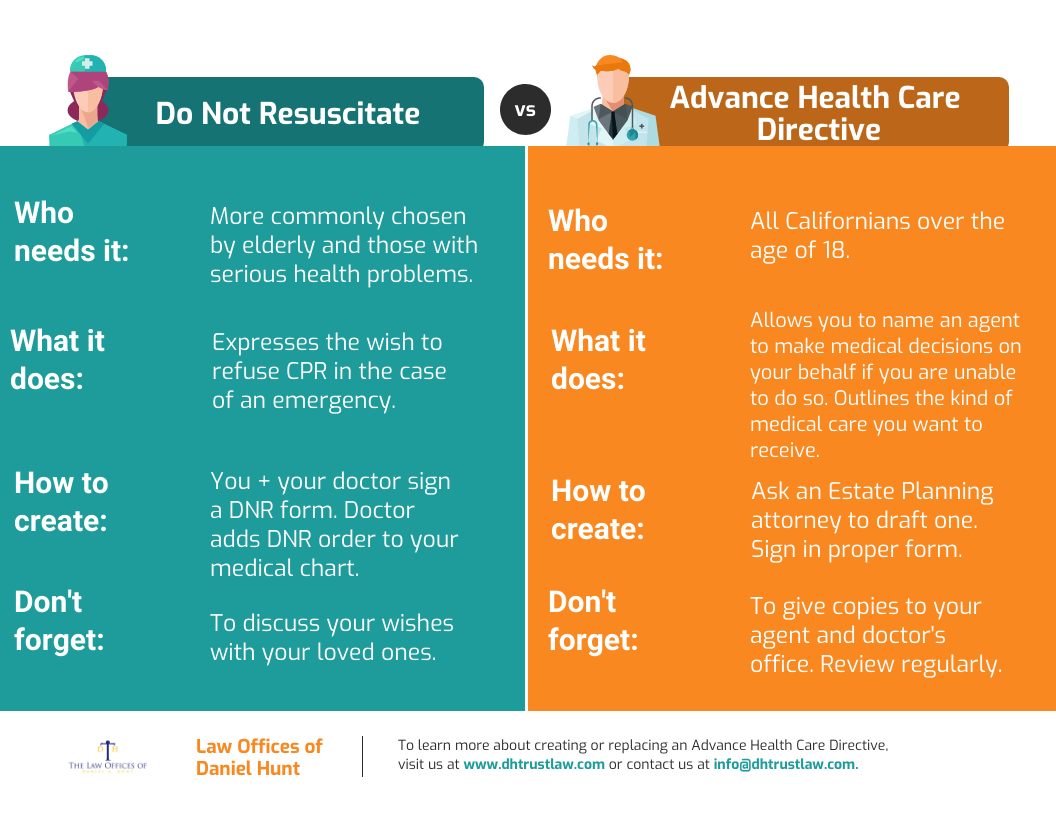
Advance medical directives, also known as living wills or healthcare directives, are legal documents that allow individuals to outline their preferences for medical treatment in case they become unable to communicate their wishes. These directives serve as a guide for healthcare providers and family members to ensure that a person’s healthcare decisions are respected and followed.
There are several key reasons why having an advance medical directive is important:
- Control Over Healthcare Decisions: By creating an advance medical directive, individuals can specify the type of care they wish to receive or refuse in various medical situations. This allows them to maintain control over their healthcare decisions even if they are incapacitated.
- Relieving Family Burden: Having a clear directive in place can relieve family members of the burden of making difficult decisions on behalf of their loved ones. It provides peace of mind knowing that the person’s wishes are being honored.
- Ensuring Personal Values Are Respected: Advance directives enable individuals to express their personal values and beliefs regarding medical treatment. This ensures that healthcare decisions align with their religious, cultural, or ethical beliefs.
- Avoiding Unwanted Treatment: With an advance medical directive, individuals can specify treatments they do not wish to receive, such as life-sustaining measures or certain procedures. This helps prevent unwanted interventions and ensures that care is provided according to their preferences.
In conclusion, advance medical directives play a crucial role in empowering individuals to make informed decisions about their healthcare even when they are unable to communicate. It is important for everyone to consider creating an advance directive to ensure that their wishes are respected and followed during times of medical incapacity.
7 Benefits of an Advance Medical Directive: Empowering Personal Healthcare Choices
- Empowers individuals to make decisions about their own healthcare.
- Ensures that personal preferences for medical treatment are respected.
- Relieves family members of the burden of making difficult healthcare decisions.
- Provides peace of mind knowing that one’s wishes will be followed in case of incapacity.
- Helps avoid unwanted or unnecessary medical interventions.
- Allows individuals to align medical care with their personal values and beliefs.
- Offers a sense of control and autonomy over future healthcare decisions.
Challenges of Advance Medical Directives: Understanding Potential Drawbacks
- May be difficult to predict all future medical scenarios and preferences accurately.
- Family members may disagree with the directives outlined in the document.
- Healthcare providers may not always adhere to the directives due to legal or ethical concerns.
- Advance directives may not cover every possible medical situation, leading to ambiguity in decision-making.
- Updating or revising advance directives can be overlooked, resulting in outdated or inaccurate instructions.
- Some individuals may feel uncomfortable or anxious discussing end-of-life care preferences, leading to reluctance in creating advance directives.
Empowers individuals to make decisions about their own healthcare.
One significant advantage of advance medical directives is that they empower individuals to make decisions about their own healthcare. By creating a directive, individuals can proactively outline their treatment preferences and healthcare choices, ensuring that their wishes are respected even if they are unable to communicate them later on. This sense of empowerment allows individuals to maintain control over their medical care and ensures that their values and beliefs guide the decision-making process, promoting autonomy and self-determination in healthcare matters.
Ensures that personal preferences for medical treatment are respected.
An important advantage of having an advance medical directive is that it ensures that personal preferences for medical treatment are respected. By clearly outlining one’s wishes regarding healthcare interventions in advance, individuals can have peace of mind knowing that their choices will be honored even if they are unable to communicate them later on. This proactively ensures that medical decisions align with their values, beliefs, and desired level of care, providing a sense of control and dignity in critical healthcare situations.
Relieves family members of the burden of making difficult healthcare decisions.
One significant benefit of having an advance medical directive is that it relieves family members of the burden of making difficult healthcare decisions on behalf of their loved ones. By clearly outlining their preferences for medical treatment in advance, individuals spare their family members from the emotional stress and potential conflicts that can arise when trying to make critical healthcare choices without clear guidance. This proactive approach allows family members to focus on providing support and comfort to their loved ones during challenging times, knowing that they are honoring the individual’s wishes as outlined in the advance directive.
Provides peace of mind knowing that one’s wishes will be followed in case of incapacity.
Having an advance medical directive provides a sense of peace of mind, knowing that one’s wishes regarding medical treatment will be respected and followed even in situations of incapacity. By clearly outlining preferences for healthcare decisions in advance, individuals can rest assured that their voice will be heard and honored, alleviating concerns about receiving care that may not align with their values or beliefs. This assurance allows individuals to focus on their well-being without the worry of their wishes being misunderstood or disregarded during critical moments.
Helps avoid unwanted or unnecessary medical interventions.
An essential benefit of having an advance medical directive is that it helps individuals avoid unwanted or unnecessary medical interventions. By clearly outlining their preferences for treatment in advance, individuals can ensure that healthcare providers respect their wishes and refrain from administering treatments that they do not desire. This proactive approach not only helps prevent unnecessary discomfort or stress but also ensures that medical care aligns with the individual’s values and preferences, promoting a more personalized and patient-centered healthcare experience.
Allows individuals to align medical care with their personal values and beliefs.
An important benefit of advance medical directives is that they enable individuals to align their medical care with their personal values and beliefs. By clearly outlining their preferences for treatment in various medical scenarios, individuals can ensure that healthcare decisions are made in accordance with their religious, cultural, or ethical beliefs. This aspect of advance directives helps individuals maintain autonomy over their healthcare decisions and ensures that their care reflects their deeply held values, providing peace of mind for both the individual and their loved ones.
Offers a sense of control and autonomy over future healthcare decisions.
An important benefit of having an advance medical directive is that it offers individuals a sense of control and autonomy over their future healthcare decisions. By outlining their preferences for medical treatment in advance, individuals can ensure that their wishes are respected and followed, even if they are unable to communicate them at a later time. This sense of control empowers individuals to make informed choices about their healthcare, providing peace of mind and reassurance that their values and preferences will guide their medical care in the future.
May be difficult to predict all future medical scenarios and preferences accurately.
One potential drawback of advance medical directives is the challenge of accurately predicting all future medical scenarios and preferences. Individuals may find it difficult to anticipate every possible medical situation they could encounter and specify their preferences with complete accuracy. This limitation can lead to ambiguity or gaps in the directive, potentially causing confusion or disagreements among healthcare providers and family members when decisions need to be made. Despite efforts to outline detailed instructions, the dynamic nature of healthcare and individual circumstances may make it challenging to cover all contingencies comprehensively in an advance directive.
Family members may disagree with the directives outlined in the document.
In some cases, a con of advance medical directives is that family members may disagree with the directives outlined in the document. This can lead to potential conflicts and emotional distress among family members, especially if there are differing opinions on the appropriate course of medical treatment. Disagreements may arise due to personal beliefs, cultural differences, or simply misunderstandings regarding the individual’s wishes. Resolving such conflicts can be challenging and may require mediation or legal intervention, highlighting the importance of open communication and clarity when creating advance directives to minimize potential disagreements among family members.
Healthcare providers may not always adhere to the directives due to legal or ethical concerns.
One significant con of advance medical directives is that healthcare providers may not always adhere to the directives due to legal or ethical concerns. While advance directives are legally binding documents, there can be situations where healthcare providers face moral dilemmas or legal uncertainties when following the specified instructions. Providers may feel conflicted if they believe that honoring the directive goes against their professional ethics or if they are unsure about the legality of certain decisions. This lack of adherence can lead to challenges in ensuring that a person’s healthcare preferences are respected and implemented as intended, highlighting a potential limitation in the effectiveness of advance medical directives.
Advance directives may not cover every possible medical situation, leading to ambiguity in decision-making.
One notable con of advance medical directives is that they may not cover every possible medical situation, which can result in ambiguity and challenges in decision-making. While individuals can outline their preferences for certain treatments or interventions in advance directives, unforeseen medical circumstances or evolving healthcare technologies may present scenarios not explicitly addressed in the directive. This lack of specificity can leave healthcare providers and family members uncertain about the appropriate course of action, potentially leading to disagreements or delays in crucial decision-making processes. It underscores the importance of regularly reviewing and updating advance directives to ensure they align with one’s current values and preferences.
Updating or revising advance directives can be overlooked, resulting in outdated or inaccurate instructions.
One significant drawback of advance medical directives is that the process of updating or revising them can often be overlooked, leading to outdated or inaccurate instructions. Changes in personal preferences, medical conditions, or healthcare options may occur over time, making it essential to regularly review and modify advance directives to reflect current wishes accurately. Failure to update these documents can result in healthcare decisions that no longer align with an individual’s desires, potentially leading to confusion and conflicts among healthcare providers and family members when critical medical decisions need to be made. Regularly revisiting and revising advance directives is crucial to ensure that they remain relevant and reflective of one’s current healthcare preferences and values.
Some individuals may feel uncomfortable or anxious discussing end-of-life care preferences, leading to reluctance in creating advance directives.
Some individuals may experience discomfort or anxiety when confronted with discussions about end-of-life care preferences, which can create a barrier to creating advance medical directives. The sensitive nature of these conversations and the emotional weight associated with making decisions about one’s own mortality can lead to reluctance in addressing such topics. This discomfort may prevent individuals from clearly articulating their healthcare wishes and may delay the process of creating advance directives, potentially leaving them unprepared for future medical situations. It is important to acknowledge and address these emotional challenges in order to encourage open communication and facilitate the creation of advance directives that truly reflect an individual’s values and preferences.