Advancing Community Wellness Through Primary Health Care Initiatives
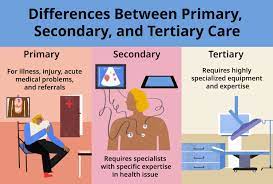
The Importance of Primary Health Care
Primary health care serves as the cornerstone of a well-functioning healthcare system, providing essential and accessible healthcare services to individuals and communities. It encompasses a range of services that promote preventive care, early intervention, and ongoing management of health conditions.
Key Components of Primary Health Care
Primary health care includes a variety of services such as:
- Preventive care, including vaccinations and screenings
- Management of chronic conditions like diabetes and hypertension
- Treatment of common illnesses and injuries
- Promotion of healthy lifestyle choices
- Mental health support and counseling
Benefits of Primary Health Care
There are numerous benefits associated with primary health care, including:
- Early detection and treatment of health issues, leading to better health outcomes
- Cost-effective care that reduces the need for expensive hospital visits or emergency room treatments
- Promotion of overall well-being through preventive measures and education
- Improved coordination of care for individuals with multiple health conditions
- Enhanced access to healthcare services for underserved populations
The Role of Primary Care Providers
Primary care providers, such as family physicians, nurse practitioners, and physician assistants, play a crucial role in delivering primary health care services. They serve as the first point of contact for patients seeking medical assistance and provide comprehensive care that addresses both physical and mental health needs.
Promoting Equity in Healthcare Through Primary Health Care
One of the key principles of primary health care is its focus on equity and social justice. By ensuring that essential healthcare services are available to all individuals regardless of their socio-economic status or background, primary health care helps reduce disparities in access to quality healthcare.
In Conclusion
Primary health care plays a vital role in promoting individual well-being, preventing diseases, and improving overall population health. By emphasizing preventive measures, early intervention, and comprehensive care, primary health care paves the way for a healthier society.
Five Key Benefits of Primary Health Care: Prevention, Early Detection, Improved Outcomes, Cost Efficiency, and Personalized Attention
- Promotes preventive care through regular check-ups and screenings
- Enhances early detection and management of health conditions
- Improves overall health outcomes by addressing health issues promptly
- Provides cost-effective healthcare solutions for individuals and communities
- Offers personalized and continuous care that focuses on individual needs
Seven Key Challenges Facing Primary Health Care: Accessibility, Timeliness, and Quality Concerns
- Limited availability of specialized services
- Long wait times for appointments with primary care providers
- Challenges in continuity of care when patients see different providers within a practice
- Potential for misdiagnosis or oversight of complex medical conditions
- Inadequate resources for mental health support and counseling
- Difficulty in accessing primary care services in rural or underserved areas
- Pressure on primary care providers to manage a wide range of health issues within limited timeframes
Promotes preventive care through regular check-ups and screenings
One of the significant advantages of primary health care is its emphasis on promoting preventive care through regular check-ups and screenings. By encouraging individuals to undergo routine health assessments and screenings, primary care providers can detect potential health issues at an early stage, allowing for timely intervention and treatment. This proactive approach not only helps prevent the development of serious illnesses but also promotes overall well-being by empowering individuals to take charge of their health through regular monitoring and preventive measures.
Enhances early detection and management of health conditions
One significant advantage of primary health care is its ability to enhance early detection and management of health conditions. By providing regular check-ups, screenings, and preventive care services, primary care providers can identify potential health issues at their earliest stages. This proactive approach allows for timely intervention, effective treatment planning, and better health outcomes for individuals. Early detection not only improves the chances of successful treatment but also helps prevent the progression of diseases, ultimately leading to a healthier population overall.
Improves overall health outcomes by addressing health issues promptly
Primary health care significantly enhances overall health outcomes by promptly addressing health issues before they escalate. By focusing on preventive care and early intervention, primary health care providers can identify and treat medical concerns in their initial stages, leading to better prognosis and reduced complications. This proactive approach not only improves individual health but also contributes to better population health by minimizing the burden of advanced and preventable diseases. Prioritizing prompt healthcare interventions through primary care services is a key factor in achieving positive and sustainable health outcomes for individuals and communities alike.
Provides cost-effective healthcare solutions for individuals and communities
Primary health care offers a significant advantage by providing cost-effective healthcare solutions for individuals and communities. By focusing on preventive care, early intervention, and management of health conditions at the primary care level, individuals can avoid costly hospital visits and emergency room treatments. This proactive approach not only saves money for individuals but also contributes to overall healthcare cost reduction for communities. Additionally, by addressing health issues early on through primary health care services, the need for expensive treatments or interventions down the line is minimized, leading to long-term cost savings and improved financial accessibility to essential healthcare services.
Offers personalized and continuous care that focuses on individual needs
Primary health care stands out for its ability to provide personalized and continuous care that prioritizes individual needs. By fostering a patient-centered approach, primary health care professionals develop a deep understanding of each person’s unique health concerns, preferences, and circumstances. This tailored care ensures that individuals receive treatments and interventions that are specifically suited to their needs, promoting better health outcomes and overall well-being. The ongoing relationship between patients and primary care providers allows for comprehensive monitoring, timely interventions, and proactive management of health issues, ultimately leading to improved quality of care and patient satisfaction.
Limited availability of specialized services
One significant drawback of primary health care is the limited availability of specialized services. While primary care providers offer essential and general healthcare services, they may lack the expertise and resources to address complex or specialized medical conditions effectively. Patients requiring specialized treatments or interventions may face challenges accessing timely care within the primary health care setting, leading to potential delays in diagnosis and treatment. This limitation underscores the importance of a well-integrated healthcare system that ensures seamless referrals to specialists when needed, to provide comprehensive and effective healthcare for all individuals.
Long wait times for appointments with primary care providers
One significant drawback of primary health care is the long wait times for appointments with primary care providers. Patients often face challenges in accessing timely healthcare services due to the high demand for primary care and limited availability of appointments. Prolonged wait times can lead to delayed diagnosis and treatment, potentially exacerbating health conditions and causing frustration for individuals seeking immediate medical attention. Addressing this issue is crucial to improving patient satisfaction and ensuring timely access to essential healthcare services.
Challenges in continuity of care when patients see different providers within a practice
One significant challenge in primary health care arises when patients see different providers within a practice, leading to issues with continuity of care. When patients interact with multiple healthcare professionals, there can be a lack of seamless coordination and communication among providers, potentially resulting in fragmented care and gaps in treatment plans. This fragmentation may hinder the establishment of a strong patient-provider relationship and impede the sharing of crucial medical information, ultimately affecting the quality and consistency of care delivered to patients. Addressing these challenges requires enhanced collaboration among healthcare team members and the implementation of robust systems to ensure effective communication and coordination across all providers within the practice.
Potential for misdiagnosis or oversight of complex medical conditions
One significant con of primary health care is the potential for misdiagnosis or oversight of complex medical conditions. Primary care providers may not always have the specialized knowledge or resources to accurately diagnose and manage intricate health issues, leading to delays in treatment or incorrect assessments. This limitation underscores the importance of timely referrals to specialists when dealing with complex medical conditions to ensure that patients receive the most appropriate and effective care for their specific needs.
Inadequate resources for mental health support and counseling
One significant con of primary health care is the inadequate allocation of resources for mental health support and counseling. Due to limited funding and prioritization of physical health services, mental health often takes a back seat in primary care settings. This shortfall can result in delayed or insufficient treatment for individuals struggling with mental health issues, leading to potential complications and poorer overall health outcomes. Addressing this gap in resources is crucial to ensuring holistic and comprehensive care for patients, underscoring the importance of integrating mental health services into primary healthcare practices.
Difficulty in accessing primary care services in rural or underserved areas
One significant challenge of primary health care is the difficulty in accessing services in rural or underserved areas. Limited healthcare infrastructure, shortage of healthcare providers, and geographical barriers often result in residents of these regions facing obstacles when seeking essential primary care services. The lack of access to timely and quality healthcare in rural or underserved areas can lead to delayed diagnosis, inadequate management of health conditions, and disparities in health outcomes for populations residing in these underserved areas. Efforts to address these access barriers through innovative solutions and targeted interventions are crucial to ensuring equitable access to primary health care for all individuals, regardless of their geographic location.
Pressure on primary care providers to manage a wide range of health issues within limited timeframes
One significant challenge of primary health care is the immense pressure placed on primary care providers to address a broad spectrum of health issues within constrained timeframes. With increasing patient loads and administrative demands, primary care providers often find themselves navigating complex medical cases while striving to deliver quality care in limited consultation times. This can lead to potential gaps in care, rushed assessments, and challenges in providing thorough treatment plans tailored to individual patient needs. The burden of managing diverse health concerns within tight schedules underscores the need for adequate support systems and resources to ensure that primary care providers can effectively meet the healthcare needs of their patients.